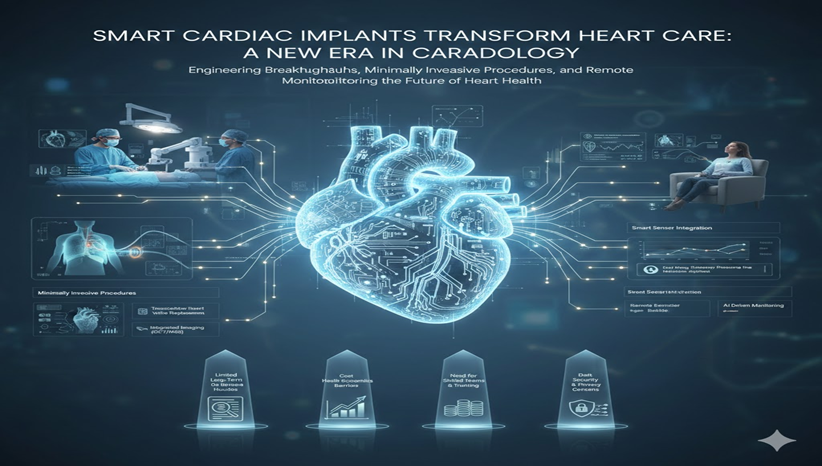
Cardiovascular disease remains a leading global health challenge. Engineers and doctors now collaborate to introduce smarter, less invasive heart-care solutions. In this context, smart cardiac implants are rising as the next frontier in cardiac treatment and monitoring. These emerging devices promise to reshape how we manage heart health. Below, I explore these advances, discuss their benefits, and highlight the challenges ahead.
Engineering Breakthroughs in Implant Design
Miniaturization and Biocompatibility
Recent engineering breakthroughs have enabled miniaturization and biocompatibility that reduce tissue trauma and improve implant longevity. For example, leadless pacemakers can now be implanted directly onto the heart wall via a catheter. These devices avoid transvenous leads, thereby lowering infection risk and simplifying recovery after implantation.
Moreover, advances in materials science have led to implants using polymers and surface coatings that encourage natural tissue integration. Such devices reduce the chance of migration or restenosis over time.
Bioresorbable and Shape-Adaptive Materials
In addition, researchers are exploring biodegradable scaffolds that serve as temporary supports. These scaffolds maintain vessel patency during healing but later dissolve, leaving only the patient’s own tissue behind. Early clinical data show these bioresorbable implants perform mechanically on par with permanent ones while minimizing long-term complications.
Furthermore, shape-memory alloys and smart materials are being developed to let implants adapt to physiological conditions. Such materials could enable devices that change shape or rigidity in response to pressure or temperature. This adaptability might improve comfort and safety over the cardiac cycle.
Minimally Invasive Procedures: A Paradigm Shift
Transitioning from design to use, these innovations now enable minimally invasive procedures that avoid open-heart surgery. For instance, transcatheter heart valve replacement is shifting the paradigm for valve disease. Clinicians can compress a prosthetic valve into a catheter, guide it through peripheral arteries, and deploy it directly at the native valve site. As a result, patients avoid sternotomy, hospital stay periods shorten, and recovery accelerates.
Additionally, modern catheters often include integrated imaging such as optical coherence tomography or near-infrared spectroscopy to visualize artery walls and plaque in real time. With this information, physicians can tailor interventions: they can assess whether plaque is calcified or lipid-rich, choose whether a vessel needs pre-dilation, and decide on the optimal implant size. This convergence of diagnostic and therapeutic functions strengthens the precision of cardiac care.
Smart Sensor Integration and Remote Monitoring
Beyond procedural improvements, the most transformative change may come from integrating smart sensors for continuous patient monitoring. Contemporary implants pacemakers, defibrillators, and hemodynamic monitors, can now embed sensors that collect data on heart-rate variability, intracardiac pressures, and electrical conduction. Through secure wireless networks, these sensors transmit data to digital platforms where clinicians can review trends and detect early warning signs of deterioration.
In chronic heart-failure care, for example, subtle rises in pulmonary pressure often precede worsening symptoms. Smart sensors can detect these early signals, alert care teams days before the patient experiences shortness of breath or fatigue. These early warnings allow medication adjustments to prevent hospitalisations. Additionally, artificial intelligence algorithms can analyse the continuous data streams to distinguish between benign fluctuations and clinically significant changes. Consequently, this union of implantable hardware and cloud-based analytics supports a shift toward proactive, personalized cardiac care.
Challenges to the Adoption of Smart Implants
- Limited Long-Term Data and Regulatory Hurdles: Despite these promising advances, some hurdles remain before smart cardiac implants become standard practice. First, long-term safety and efficacy data are still limited, especially for implants using bioresorbable materials or AI-driven systems. Regulatory agencies often require extensive trials, which can slow down adoption.
- Cost and Health-Economics Barriers: Second, cost and health economics play a significant role. Hospitals and insurers need clear evidence that advanced devices actually reduce overall costs through fewer readmissions, shorter procedures, or improved quality of life. Until such evidence accumulates, widespread adoption may face financial barriers.
- Need for Skilled Teams and Training: Third, sophisticated devices require skilled teams. Physicians, nurses, and technicians must acquire new competencies to implant and manage such devices. Accordingly, many medical training programs are integrating simulation-based workshops and fostering interdisciplinary collaboration. Without proper training, even the best devices may fail to deliver optimal outcomes.
- Data Security and Privacy Concerns: Finally, as more patient data flows through digital networks, data security and privacy become critical. Healthcare institutions, device manufacturers, and software developers must coordinate to build robust encryption, privacy safeguards, and interoperability standards. Otherwise, patients’ sensitive health information could be vulnerable.
Conclusion
Smart cardiac implants represent a remarkable leap forward. They combine miniaturized hardware, biocompatible materials, and digital connectivity to deliver safer, more personalized, and less invasive cardiac care. With continuous monitoring and remote diagnostics, they can detect potential problems early and enable timely interventions.
However, realizing this vision depends on thorough long-term testing, cost-benefit validation, skilled medical teams, and strong data security frameworks. With careful investment and collaboration among engineers, clinicians, regulators, and payers, smart implants could indeed reshape cardiology. Ultimately, these devices have the potential to help millions live longer and healthier lives with fewer hospital visits and better peace of mind.